We use cookies to make your experience better. To comply with the new e-Privacy directive, we need to ask for your consent to set the cookies. Learn more.
TWO TYPES OF SOUND WAVES
Extracorporeal shockwave therapy (ESWT) technology encompasses the use of two distinct forms of sound waves to transfer energy into tissue, resulting in two types of shockwave devices that clinicians can choose to incorporate into their practice.
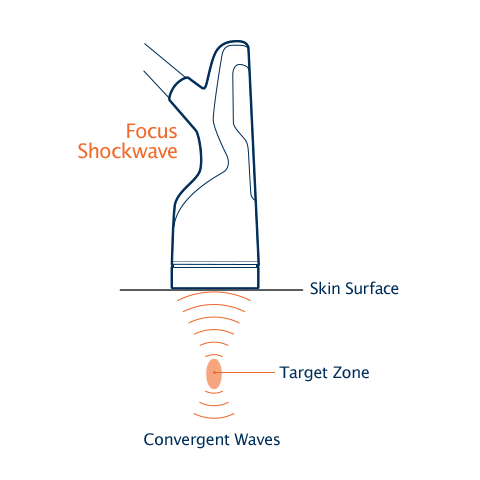
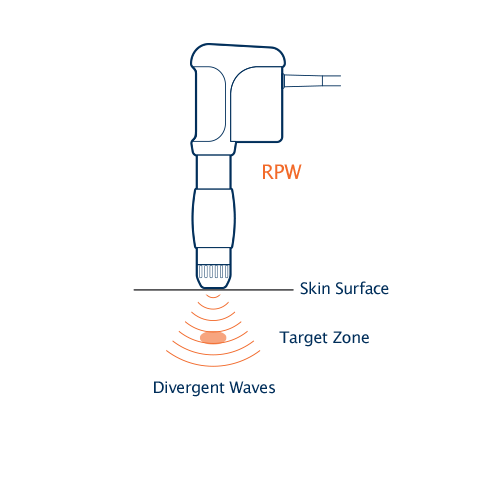
Focus Shockwaves vs. Radial Pressure Waves
The Chattanooga® Focus Shockwave device generates sound waves via an electromagnetic hand piece with a built-in water buffer, while the Radial Pressure Wave devices utilize a pneumatic/ballistic design. These differences impact the waveforms they produce.13,14
Focused shockwaves have higher peak energy and generate maximal force at a selected depth16. Radial pressure wave devices generate their maximal energy on the skin, which then dissipates as it travels to depth15. Energy levels at depth are dictated by the settings on the machine and the applicator used.
Treatment Applications
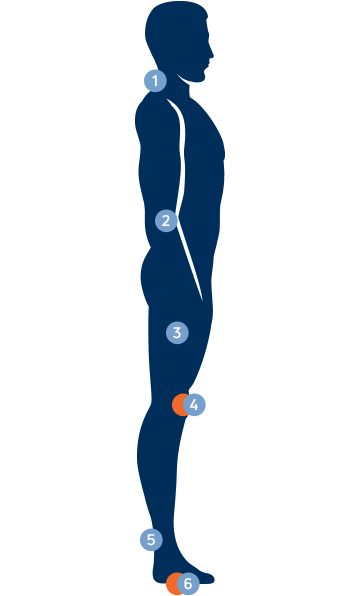
Treatment is performed directly on the skin, but is non-invasive. The time alloted for a specific treatment will depend on the area and depth of the tissue being treated. This will normally fall within 2-4 minutes per area treated.
Benefits:
- Short treatment time (a few minutes)
- Precise and targeted application
- Results in a few treatments
- Non-invasive technology
- Alternative to medication
- Myofascial trigger points
- Disorders of tendons insertions
- Pulse vibration massage
- Pain and inflammation in orthopaedic conditions
- Pulse vibration massage
- Plantar fasciitis
Pathologies
Achilles tendinopathy is a common condition characterized by pain, stiffness, and swelling in the Achilles tendon, typically resulting from overuse, poor biomechanics, or inadequate recovery following physical activity. The condition can be classified into two types: insertional tendinopathy (where the tendon attaches to the heel bone) and mid-portion tendinopathy (occurring higher up the tendon). Achilles tendinopathy affects approximately 2-3 per 1,000 people annually in the general population. It is a significant issue among athletes, particularly those involved in activities that require running and jumping.
Symptoms include:
- Pain and stiffness in the Achilles tendon, particularly in the morning or after periods of inactivity.
- Swelling and thickening of the tendon.
- Pain that worsens with activity, especially running or jumping.
- Limited range of motion in the ankle.
Causes of Achilles Tendinopathy
Achilles tendinopathy is primarily a result of mechanical overload or repetitive microtrauma to the Achilles tendon. Several factors contribute to the onset and progression of this condition, including intrinsic tendon-related factors, extrinsic factors related to activity and training, and systemic conditions:
- Repetitive Overuse and Mechanical Load, such as Chronic overload or sudden increase in activity
- Biomechanical Abnormalities, including abnormal foot mechanics, leg length discrepancies and poor ankle dorsiflexion
- Age-related degeneration including tendon degeneration or creased healing capacity
- Training Errors and Inappropriate footwear
- Previous Injury and Tendon Weakness

Interventions
Treatment Options include Physical Therapy, exercises and conservative treatments. Medical and Surgical Modalities such as (NSAIDs), Corticosteroid Injections or Platelet-Rich Plasma (PRP) Therapy can be recommended as part of a treatment plan. Prolotherapy involves injecting an irritant solution, typically dextrose, into the tendon to stimulate the body’s healing response. The goal is to promote tissue regeneration and strengthen the tendon over time.
Shockwave Therapy
There are a variety of studies supporting the use of ESWT in the treatment of Achilles tendinopathy. A study by Stania et al (2023) aimed to subjectively and objectively determine the therapeutic efficacy of radial shock wave therapy (RSWT) and ultrasound (US) therapy in non-insertional Achilles tendinopathy. The findings were that RSWT provided significantly greater improvement of VISQA-A scores than US therapy and also more efficient postural control in standing. Paantjens et al (2022) carried out a systematic review of Randomised Control Trials to consider the outcomes of using Shockwave Therapy for both mid portion and Insertional Achilles tendinopathies. The findings showed that there is moderate evidence supporting the effectiveness of Shockwave Therapy in addition to a tendon loading program in mid-portion tendinopathies. Evidence supporting the effectiveness of Shockwave Therapy for Insertional Achilles Tendinopathies is still unclear.
Click HERE to see more info on Shockwave Therapy
Lightforce Laser Therapy
This has been shown to be very effective in addressing pain and improving function in a variety of conditions. A study by Tumilty at al (2016) considered the use of High Intensity PBMT when combined with eccentric exercise for Achilles Tendinopathy. The conclusion was that the best results were obtained when a combined protocol of twice a week eccentric exercise plus high intensity PBMT were prescribed.
Click HERE to see more info on Lightforce Laser Therapy
Ultrasound Therapy
Therapeutic ultrasound is used to deliver sound waves to the Achilles tendon, which can help increase blood flow and reduce inflammation, promoting faster healing. Ultrasound therapy is often combined with other treatments, such as stretching and strengthening exercises.
Click HERE to see more info on Ultrasound Therapy
Rotator cuff tendinopathy is a common condition affecting the shoulder, especially in individuals who perform repetitive overhead movements or participate in activities that place stress on the shoulder joint. It is a type of rotator cuff injury that involves inflammation, degeneration, or tearing of the tendons in the rotator cuff, a group of four muscles and their associated tendons that stabilize the shoulder. In contrast a frozen shoulder (also known as adhesive capsulitis) is a condition characterised by a dull or aching pain with limited range of motion (ROM).
Symptoms include:
- A dull deep shoulder ache
- Pain that disturbs sleep
- Swelling in the shoulder area
- Limitation or discomfort with overhead movement and with moving the arm behind the back
- Arm weakness
- If left untreated, rotator cuff tendinitis can worsen and lead to a partially or completely torn tendon
Causes of Rotator Cuff Tendinopathy
- Repetitive overhead movements making rotator cuff injuries common across a diverse patient population.
- Trauma such as falls, rapid humeral deceleration with throwers, or high resistive forces applied through the shoulder.
- Individuals over the age of 60 are more prone to rotator cuff injury.
- Subacromial bone spurs can contribute to impingement, leading to an increased likelihood of rotator cuff pathology.
- Weakness or imbalance of muscles surrounding the shoulder joint.

Interventions
Treatment options include conservative treatments, physical therapy and strengthening exercises. Dry Needling and Acupuncture can be used to release tension, improve blood flow and provide pain relief in some cases of rotator cuff tendinopathy. Medical and Surgical Modalities such as NSAIDs, Corticosteroid Injections and/or Platelet-Rich Plasma (PRP) Therapy can be recommended as part of a treatment programme.
Shockwave Therapy (ESWT)
ESWT (Extracorporeal Shockwave Therapy), also known as Radial Shockwave (RSW) therapy, is a non-invasive treatment option that has support in the literature for helping address muscle aches and pains associated with shoulder dysfunction. During treatment with ESWT, high-energy sound waves are transmitted into the tissue propagating radially and creating a therapeutic effect on the impacted areas. Xue et al (2024) in their systematic review of 16 Randomised Control Trials (1093 patients) showed that the current evidence supports the effectiveness of Shockwave Therapy for the clinical efficacy of shoulder pain and functional recovery in patients with Rotator Cuff Tendinopathy. Shockwave Therapy provides better pain relief, functional recovery, and maintenance compared with controls.
Shao et al (2023) demonstrated a five week course of Shockwave Therapy and exercise more effectively reduced early shoulder pain than rehabilitation alone and accelerated proximal supraspinatus tendon healing at the suture anchor site after Rotator Cuff repair.
Click HERE to see more info on Shockwave Therapy
Lightforce Laser Therapy
This systematic review and meta-analysis (Hao et al 2024) aimed to identify, critically appraise, and summarize the effects of high-intensity laser therapy on subacromial impingement syndrome. The authors concluded that high-intensity laser therapy is an effective treatment for subacromial impingement syndrome to augment conventional rehabilitation protocol and optimize therapeutic outcomes. They added that rehabilitation professionals and policymakers should increase their awareness of high-intensity laser therapy as an emerging technology that may facilitate greater outcomes than current widespread standards.
Yilmaz et al 2022, also demonstrated the effectiveness of high intensity laser therapy on pain, range of motion, functional capacity, quality of life, and muscle strength in subacromial impingement syndrome in this 3-month follow-up, double-blinded, randomized, placebo-controlled trial.
Click HERE to see more info on Lightforce Laser Therapy
Plantar fasciitis is a common condition that causes heel pain due to inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of the foot and connects the heel bone to the toes. Plantar fasciitis is one of the most common causes of heel pain. It is estimated to affect about 1 in 10 people at some point during their lifetime. It is common in athletes, particular runners, due to repetitive stress on the feet. Obesity is a significant risk factor because excess weight increases stress on the plantar fascia.
Symptoms include:
Symptoms include sharp, stabbing pain in the heel, particularly with the first steps in the morning, pain that worsens after long periods of standing or rising for sitting, or pain that typically decreases with activity (but may return after prolonged standing or exercise).
Plantar fasciitis is primarily caused by repetitive mechanical stress on the plantar fascia, leading to microtears and inflammation. Key etiological factors include:
- Overuse and Repetitive Strain: Activities that place excessive stress on the plantar fascia, such as running, dancing, or prolonged standing, can overload the tissue.
- Foot Biomechanics: Abnormal foot mechanics, including overpronation (excessive inward rolling of the foot), flat feet, or high arches, can alter the distribution of force across the foot, increasing strain on the plantar fascia.
- Age-Related Changes: Degenerative changes in the plantar fascia with aging, particularly in individuals over 40, can contribute to a decreased ability to absorb shock, making the fascia more susceptible to injury.
- Obesity: Increased body mass puts additional stress on the plantar fascia, increasing the risk of developing inflammation and pain, especially in individuals with underlying structural abnormalities.
- Improper Footwear: Shoes lacking proper arch support, cushioning, or flexibility, especially when worn for long periods, can exacerbate the strain on the plantar fascia. Heel height and shoe design also play a role in altering foot mechanics.
- Tightness of Adjacent Structures: Tight calf muscles, Achilles tendinopathy, or limited ankle dorsiflexion can increase tension on the plantar fascia, further exacerbating the condition.
- Occupational Factors: Jobs that require standing for prolonged periods or involve repetitive impact (e.g., factory workers, teachers, retail workers) are associated with higher risk due to prolonged loading of the foot.
- Inflammatory or Systemic Conditions:Conditions such as rheumatoid arthritis, ankylosing spondylitis, and reactive arthritis can predispose individuals to plantar fasciitis through inflammation and altered biomechanics.

Interventions
There are many conservative treatments and at-home modalities for plantar fasciitis.
Orthotics and footwear modifications can alleviate pressure on the plantar fascia, whilst night splints hold the foot in a dorsiflexed position, keeping the plantar fascia stretched and preventing morning stiffness.
Physical therapy and exercises can address the specific causes of plantar fasciitis.
Medical and Surgical Modalities such as (NSAIDs), Corticosteroid Injections, Platelet-Rich Plasma (PRP) Therapy and Surgery (in Severe Cases) can be recommended as part of a treatment plan.
Therapeutic ultrasound uses sound waves to increase blood flow and promote healing in the plantar fascia. This modality is often used in combination with other treatments, such as physical therapy, to speed up recovery.
Shockwave Therapy (ESWT)
A study by Morrissey et al (2021) considered the efficacy of nine of the most popular interventions for Plantar Fasciitis based on Evidence Based Practice. The aim was to provide a Best Practice guide for treating Plantar Fasciitis. The published literature is dominated by systematic reviews, guidelines and meta-analyses that include low-quality trials with small sample sizes, which may inflate effect sizes and lead to incorrect interpretation. Following a mixed-method design including systematic review, expert interviews and patient survey:
- There was good agreement between the systematic review findings and interview data about taping and plantar fascia stretching for first step pain in the short-term.
- Clinical reasoning advocated combining these interventions with education and footwear advice as the core self-management approach.
- There was good expert agreement with systematic review findings recommending stepped care management with focused shockwave for first step pain in the short-term, medium-term and long-term and radial shockwave for first step pain in the short-term and long-term
- We found good agreement to 'step care' using custom foot orthoses for general pain in the short-term and medium-term.
Click HERE to see more info on Shockwave Therapy
Osteoarthritis (OA) is the most common form of arthritis, characterized by the progressive degeneration of joint cartilage and underlying bone. It commonly affects weight-bearing joints such as the knees, hips, and spine, but can also affect the hands, wrists, and other joints. It's estimated that around 10% of men and 18% of women aged 60 years and older have symptomatic osteoarthritis. By age 65, nearly 30% of people have osteoarthritis, and by age 85, the prevalence increases to around 80%.
The clinical presentation of OA varies depending on the joint involved and the severity of cartilage damage.
Symptoms include:
The primary signs and symptoms of OA include:
- Pain: Joint pain is the hallmark of OA, typically exacerbated by activity or weight-bearing and relieved by rest.
- Stiffness: Can occur in a morning or after periods of inactivity and improves with activity. Stiffness often results in reduced ROM (range of motion).
- Swelling: May occur due to synovial fluid accumulation or inflammation around the joint.
- Crepitus: The sensation or audible sound of grating or crunching (known as crepitus), is commonly felt or heard during movement of the affected joint.
- Joint Instability: Related to functional impairment (a feeling of joint instability or “giving way”) or muscle weakness.
- Decreased Function: OA can cause significant interference with daily activities. Pain, stiffness and weakness all contribute to decreased function.
Risk Factors include age, gender, obesity, joint injuries, genetics and occupational hazards.

Interventions
A combination of physical therapy and exercise will be an essential part of the recommendation for managing and treating osteoarthritis. TENS units are often used for short term pain relief and can be applied at home.
Medical and Surgical Modalities such as NSAIDs, Acetaminophen, Topical Analgesics and Corticosteroid/ Hyaluronic Acid Injections maybe prescribed for treating osteoarthritis.
Lightforce Laser Therapy
There is justifiably growing interest in the use of Photobiomodulation (PBMT) therapy (Laser) for the treatment of osteoarthritis. The therapeutic effects of PBMT in improving pain and function have been widely supported in research studies. More recently research emphasis has moved to High Intensity (HI) PBMT from Low laser therapy. A study by Poenaru et al (2024), compared the two and demonstrated much better results with the HI PBMT for decreasing pain and improving function for Knee Osteoarthritis. Stating that the analgesic effect is rapid, cumulative and long lasting.
A meta-analysis by Khalilizad et al (2024) found that High Intensity PBMT combined with exercise showed significant improvement in outcomes for both pain and improved knee function for Knee Osteoarthritis (KOA) patients. A further systematic review and meta-analysis by Cai et al (2023), compared HI PBMT to other interventions for KOA. These included: other laser therapies, conventional therapies or exercise. The authors concluded that HI PBMT should be recommended for pain relief in patients with KOA over other treatments.
Click HERE to see more info on Lightforce Laser Therapy